Rare clotting factor deficiencies are bleeding disorders in which one or more of the other clotting factors (i.e. factors I, II, V, V+VIII,VII, X, XI, or XIII) is missing or not working properly. Less is known about these disorders because they are diagnosed so rarely. In fact, many have only been discovered in the last 40 years.
How Does Clotting Work Normally?
Blood is carried throughout the body in a network of blood vessels. When tissues are injured, damage to a blood vessel may result in leakage of blood through holes in a vessel wall. The vessels can break near the surface, as in the case of a cut. They can also break deep inside the body, causing a bruise or an internal haemorrhage. Clotting, or coagulation, is a complex process that makes it possible to stop injured blood vessels from bleeding. As soon as a blood vessel wall breaks, the components responsible for coagulation, come together to form a plug at the break. Coagulation factors (coagulation proteins) are required to hold the plug (or homeostatic plug) in place and form the permanent clot and there are several steps involved in forming this plug.
Figure 1 show the four steps involved in forming a plug:
Step 1: The blood vessel is damaged
Step 2: The blood vessels contract to restrict the blood flow to the damaged area
Step 3: Blood platelets, which are very tiny cell fragments, are the first to arrive at the damaged area. The platelets stick to the walls of damaged vessles and spread out, which is called platelet adhesion. These platelets then emit chemical signals that activate other nearby platelets so that they clump together at the site of the damage in order to form a plug, the homeostatic plug. This is called platelet aggregation.
Step 4: The surface of these activated platelets forms a base on which blood coagulation can take place. the coagulation factors (or coagulation proteins) circulating in the blood are activated at the surface of the platelets to form a fibrin clot which looks something like a mesh. This is the permanent clot.
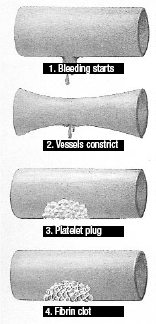
Figure 1: Forming a Clot
These factors (Factors I, II, V, VIII, IX, X, XI, XII and XIII) are triggered in a kind of domino effect, a chain reaction that is called the coagulation cascade. The following diagram shows the stages in clot formation in a way that makes it easier to understand the clotting cascade (see Figure 2).
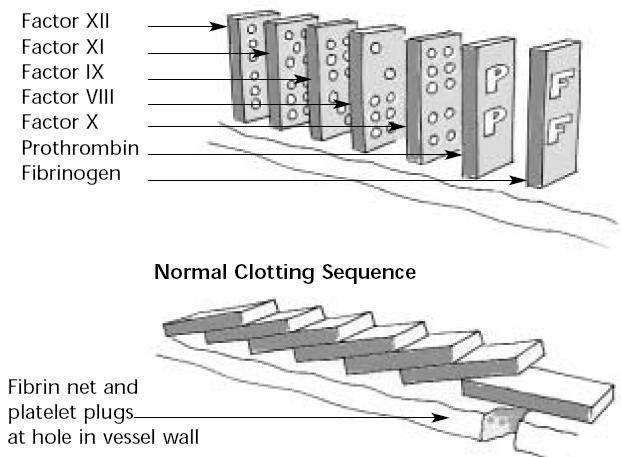
Figure 2: Domino Effect of Clotting Cascade
How Are Bleeding Disorders Inherited?
Bleeding disorders are generally passed from parent to child at the time of conception. Each cell of the body contains structures called chromosomes. A chromosome is a long chain of chemicals known as DNA. This DNA is arranged into about 30,000 units called genes. These genes determine such things as the colour of a person’s eyes. In the case of factor deficiencies, one of these genes has a defect. The defective gene that causes a factor deficiency is usually on a chromosome, which does not decide the sex of the child. This means the bleeding disorder is an autosomal inherited pattern and can affect females as well as males. The majority of bleeding disorders have an autosomal inheritance patterns. These are I, II, V, VII, X, XI, XII, XIII, vWD and Platelet function disorders.
Autosomal Inherited Bleeding Disorders
There are two types of autosomal inheritance patterns, autosomal recessive and autosomal dominant. Autosomal dominant means that only one defective gene, from one of the child’s parents is required for the disorder to affect the child. Autosomal recessive means that each parent must pass on a defective gene for the child to manifest the disorder. When only one of the two parents is a carrier of the gene responsible for the specific factor and it is passed on to a child, the child will not be affected. A carrier is someone who carries the defective gene without being affected by the disorder. For a person to be affected by specific factor deficiency, he or she must have inherited two defective genes, one from the mother and one from the father. Both parents must therefore be carriers. If a person inherits the defective gene from only one of the parents, he/she will be a carrier. His/her specific factor level will be lower than normal. Symptoms of the disease may be absent or only slightly present. Most bleeding disorders have an autosomal recessive inheritance pattern. The five illustrations below show how a factor deficiency can be passed on for each pregnancy with autosomal inherited bleeding disorders.
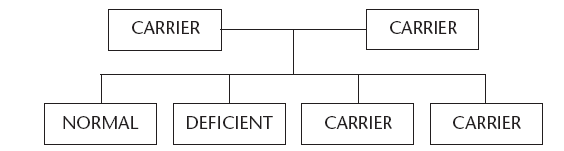
Figure 3 shows what can happen when both parents are carriers. There is one chance that the child will be normal, one chance that it will have the disorder, and there are two possibilities that the child will be a carrier.
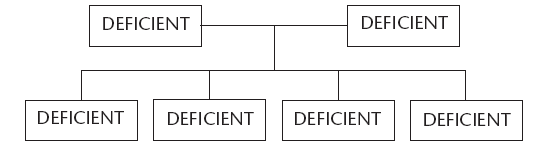
Figure 4 shows what can happen when both parents have a defective gene deficiency. All their children will also have the same deficiency.
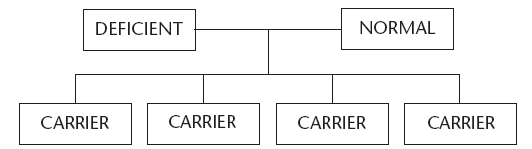
Figure 5 shows what can happen when one of the parents has the disorder and the other is normal. All their children will be carriers of the specific factor deficiency.
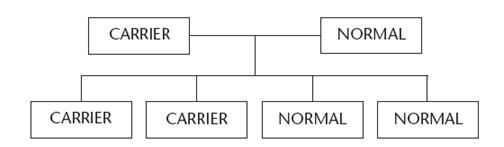
Figure 6 shows what can happen when one of the parents is a carrier and the other is normal. There are two possibilities that the child will be a carrier and two possibilities that it will be normal.
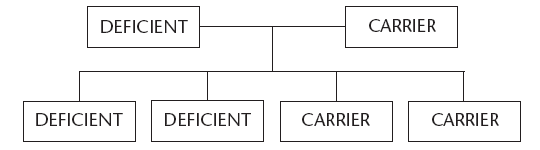
Figure 7 shows what can happen when one of the parents has the disorder and the other is a carrier. There are 2 possibilities that the child will have the disorder and 2 possibilities that it will be a carrier.
Note: Some of these rare bleeding disorders (II, X, XIII, BSS) have another form of the deficiency that is not inherited (from birth) but is acquired. There are various causes. These bleeding disorders are also extremely rare.