Clotting factors are proteins in the blood that control bleeding. When a blood vessel is injured, the walls of the blood vessel contract to limit the flow of blood to the damaged area. Then, small blood cells called platelets stick to the site of injury and spread along the surface of the blood vessel to stop the bleeding. At the same time, chemical signals are released from small sacs inside the platelets that attract other cells to the area and make them clump together to form what is called a platelet plug.
On the surface of these activated platelets, many different clotting factors work together in a series of complex chemical reactions (known as the coagulation cascade) to form a fibrin clot. The clot acts like a mesh to stop the bleeding.
Coagulation factors circulate in the blood in an inactive form. When a blood vessel is injured, the coagulation cascade is initiated and each coagulation factor is activated in a specific order to lead to the formation of the blood clot. Coagulation factors are identified with Roman numerals (e.g. factor I or FI).
What are rare clotting factor deficiencies?
If any of the clotting factors are missing or are not working properly, the coagulation cascade is blocked. When this happens, the blood clot does not form and the bleeding continues longer than it should.
Deficiencies of factor VIII and factor IX are known as haemophilia A and B, respectively. Rare clotting factor deficiencies are bleeding disorders in which one or more of the other clotting factors (i.e. factors I, II, V, VII, X, XI, or XIII) is missing or not working properly. Less is known about these disorders because they are diagnosed so rarely. In fact, many have only been discovered in the last 40 years.
How does clotting work normally?
Blood is carried throughout the body in a network of blood vessels. When tissues are injured, damage to a blood vessel may result in leakage of blood through holes in a vessel wall. The vessels can break near the surface as in the case of a cut. They can also break deep inside the body, causing a bruise or an internal haemorrhage. Clotting or coagulation is a complex process that makes it possible to stop injured blood vessels from bleeding. As soon as a blood vessel wall breaks, the components responsible for coagulation, come together to form a plug at the break. Coagulation factors (coagulation proteins) are required to hold the plug (or homeostatic plug) in place and form the permanent clot and there are several steps involved in forming this plug.

Figure 1 shows the four steps involved in forming a plug
Step 1: The blood vessel is damaged.
Step 2: The blood vessels contract to restrict the blood flow to the damaged area.
Step 3: Blood platelets, which are very tiny cell fragments, are the first to arrive at the damaged area. The platelets stick to the walls of damaged vessels and spread out, which is called platelet adhesion. These platelets then emit chemical signals that activate other nearby platelets so that they clump together at the site of the damage in order to form a homeostatic plug. This is called platelet aggregation.
Step 4: The surface of these activated platelets forms a base on which blood coagulation can take place. The coagulation factors (or coagulation proteins) circulating in the blood are activated at the surface of the platelets to form a fibrin clot which looks something like a mesh. This is the permanent clot.
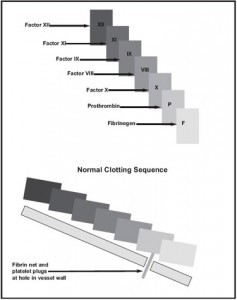
These factors (Factors I, II, V, VIII, IX, X, XI, XII and XIII) are triggered in a kind of domino effect, a chain reaction that is called the coagulation cascade. The following diagram shows the stages in clot formation in a way that makes it easier to understand the clotting cascade (See Figure 2).
How are rare bleeding disorders inherited?
Bleeding disorders are generally passed from parent to child at the time of conception. Each cell of the body contains structures called chromosomes. A chromosome is a long chain of chemicals known as DNA. This DNA is arranged into about 30,000 units called genes. These genes determine such things as the colour of a person’s eyes. In the case of factor deficiencies, one of these genes has a defect. The defective gene that causes a factor deficiency is usually on a chromosome, which does not decide the sex of the child. This means the bleeding disorder is an autosomal inherited pattern and can affect females as well as males. The majority of bleeding disorders have an autosomal inheritance pattern. These are I, II, V, VII, X, XI, XII, XIII, vWD and platelet function disorders.
Autosomal Inherited Bleeding Disorders
There are two types of autosomal inheritance patterns, autosomal recessive and autosomal dominant. Autosomal dominant means that only one defective gene, from one of the child’s parents, is required in order for the disorder to affect the child. Autosomal recessive means that each parent must pass on a defective gene in order for the child to manifest the disorder. When only one of the two parents is a carrier of the gene responsible for the specific factor and it is passed on to a child, the child will not be affected. A carrier is someone who carries the defective gene without being affected by the disorder. In order for a person to be affected by specific factor deficiency, he or she must have inherited two defective genes, one from the mother and one from the father. Both parents must, therefore, be carriers. If a person inherits the defective gene from only one of the parents, he/she will be a carrier. His/her specific factor level will be lower than normal. Symptoms of the disease may be absent or only slightly present. The majority of bleeding disorders have an autosomal recessive inheritance pattern.